The inflammatory-degenerative process in the knee joint, or gonarthrosis, occurs for various reasons. It has a very negative impact on a person's quality of life, sometimes leading to disability. How to treat arthrosis of the knee joint and prevent complications?
What is arthrosis?
About 22% of the world's population suffers from gonarthrosis, and women are more often affected. This dangerous disease is characterized by rapid development.
If treatment is not started on time, the knee joint may completely collapse. This leads to impaired musculoskeletal function. Movement can only be done with the help of crutches, or the person becomes hostage to a wheelchair.
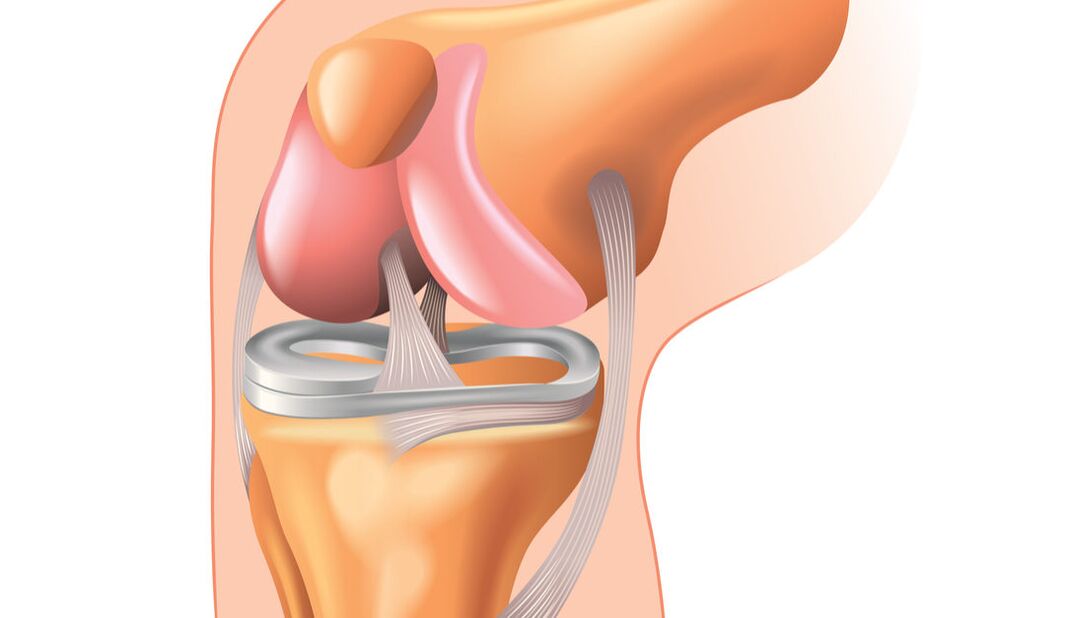
The knee joint is the second largest, after the hip, and the most complex structure. It allows you to bend and straighten your legs in different directions, promoting correct body position and coordination in space. These are strong and stable joints that can support a person's weight. Consists of 3 bones: femur, tibia and fibula, as well as the patella or kneecap. Includes osteochondral structures, muscles, ligaments, and nerve fibers.
This disease begins with a violation of blood circulation and joint tissue nutrition. First of all, cartilage suffers. The quality and quantity of synovial fluid, which is located in the joint capsule and contributes to the smooth functioning of the knee, decreases. Friction occurs between joint parts. Gradually, the cartilage cracks and collapses. Unprotected bones begin to rub against each other. Pain occurs and a throbbing sound is heard.
Cause of disease
It mainly affects older people, especially women who are overweight. As a result of hormonal changes, the cartilage in the knee is very worn. Gonarthrosis to varying degrees, after 60 years, occurs in more than 80% of people.
There are other reasons for the appearance of knee arthrosis:
- congenital joint pathology;
- dysplasia;
- injuries, operations;
- removal of the meniscus or part of it;
- arthritis;
- lumbar spine disease;
- hormonal disorders;
- low metabolism.
The risk of developing this disease increases in people involved in repetitive physical labor. This group also includes athletes, people who lead a sedentary lifestyle, and people with poor environmental conditions. Often patients are people who are dependent on toxic substances (drugs, alcohol, smoking).
The cause of joint deformation may be due to work associated with continuous hypothermia. The provoking factor is the period after menopause, when a woman experiences gynecological disorders (fibroadenoma, endometriosis, uterine fibroids). Due to the lack of minerals and vitamins in the body, diet can be a trigger.
Stages and symptoms
Gonarthrosis can be unilateral or bilateral. According to the nature of the manifestation, the disease is divided into degrees:
- At this stage, there are no obvious clinical signs. There may be some discomfort and pain after prolonged exercise, which disappears after rest. The pain is felt in the morning, when moving, it disappears after some time. Stage 1 arthrosis is rarely diagnosed, incidentally, during a routine examination.
- Pain and stiffness in the knee increases. Someone saved his leg and tried to lighten his load. As a result, the muscles atrophy, the joint changes shape, formation can be felt, and the leg at the knee does not fully extend.
- Constant pain. The legs are not straight or bent, and it is difficult for the person to walk. Partial or complete loss of movement develops. Cartilage is completely destroyed, friction between the bones of the joint increases with the formation of osteophytes.
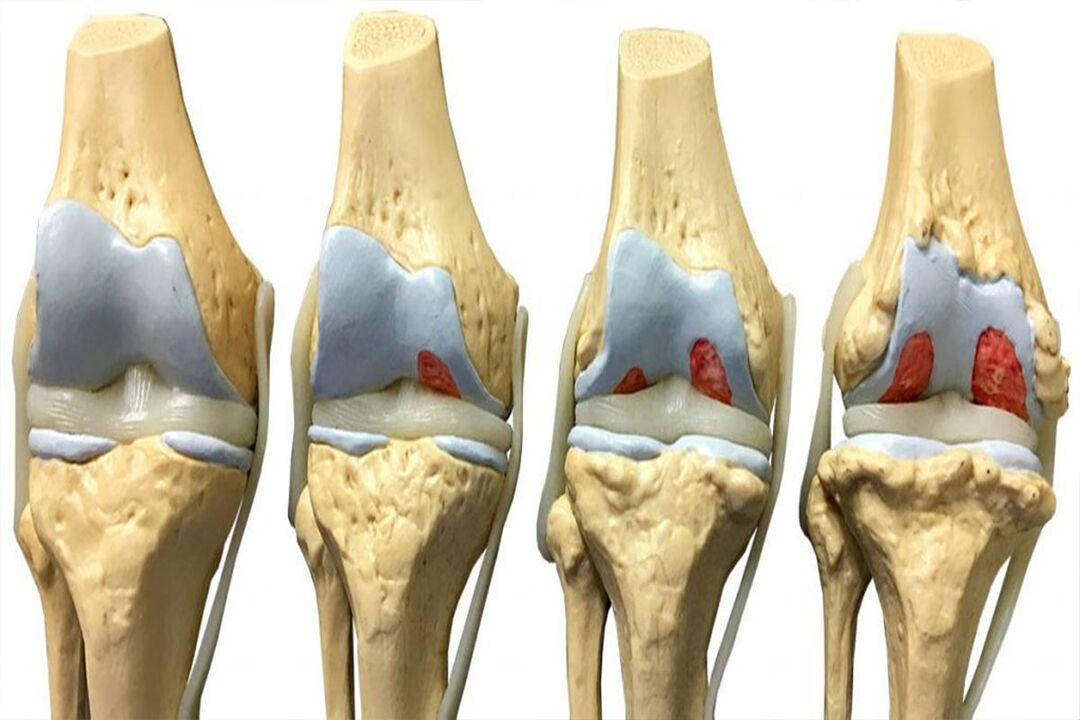
In addition to pain in grades 2 and 3, a throbbing sound is heard in the knee. Fluid and pieces of cartilage tissue can accumulate in the joint capsule, leading to swelling. At the final stage, the inflammatory process is pronounced, the knee joint is deformed.
Diagnostics
If you have knee pain, you can contact your local doctor, who, if necessary, will refer you to an orthopedist, traumatologist, rheumatologist or endocrinologist.
To find out the cause and treatment of gonarthrosis, a comprehensive diagnosis is required:
- general blood and biochemical tests;
- rheumatic test;
- radiography;
- Ultrasound and MRI can detect the disease at an early stage;
- arthroscopy.
X-ray allows you to see the condition of the cartilage and changes in the bones in stages 2 and 3. These are narrowing of the joint space, osteophytes along the edge of the patella, changes in the periosteum. Arthroscopy provides more detailed information about the meniscus, synovial membrane, and the presence of fluid. This method is also used in knee treatment, to remove pieces of cartilage or meniscus.
Treatment of knee arthrosis
Therapy is long and sometimes painful. Having appeared once, the disease reminds itself for the rest of your life. The main drugs used for treatment are non-steroidal anti-inflammatory drugs. Most often these are drugs based on non-steroidal anti-inflammatory drugs (NSAIDs) from the group of phenylacetic acid derivatives. They relieve inflammation and pain. Medicines are relatively cheap, but lead to the formation of ulcers and erosion of the stomach and duodenum. Modern drugs cause fewer side effects, but are expensive.
Treatment measures for stage 1 include exercise-related preventive measures. Daily exercise, the use of contrast showers, the swimming pool 2 times a week, and the fight against weight gain are required.
Stage 2 requires joint fixation - the use of elastic bandages, bandages or orthoses. To relieve pain, NSAIDs are used in the form of creams and ointments. To reduce the level of cartilage destruction, patients are given drugs from the group of chondroprotectors.
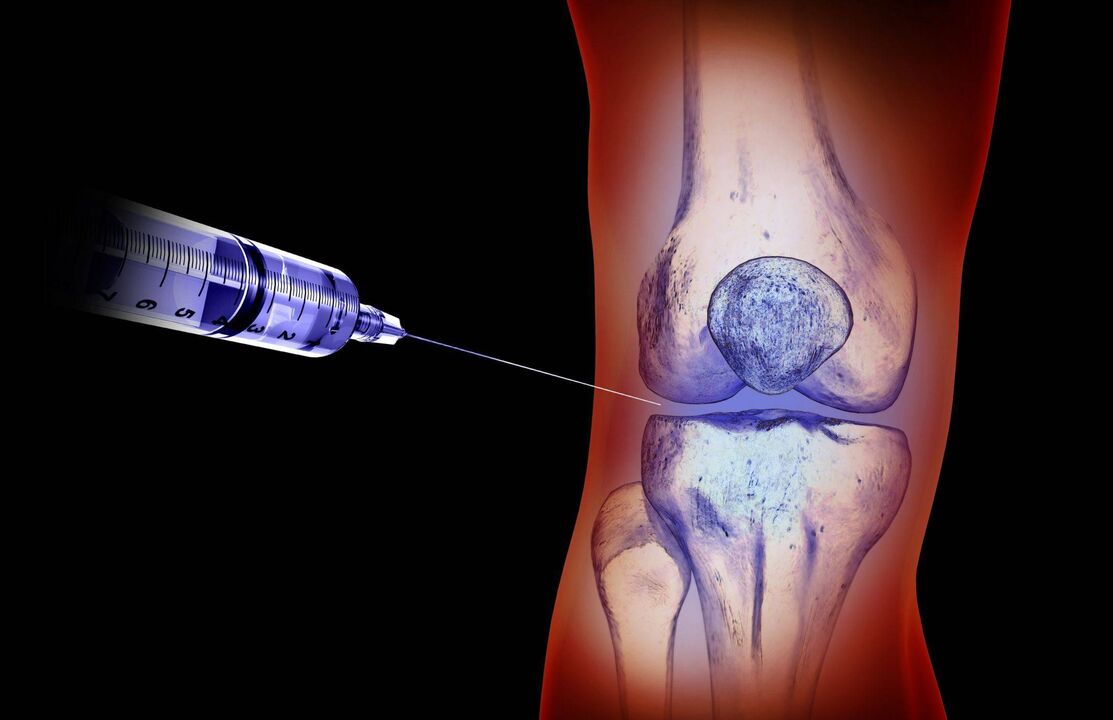
Severe severity requires oral administration of NSAIDs. Intra-articular injections of hormonal drugs are indicated - synthetic glucocorticosteroids (GCS), which have high glucocorticosteroid and low mineralocorticosteroid activity. In addition, painkillers are prescribed.
Hyaluronic acid solution is injected into the joint. It is a substitute for intra-articular fluid and nourishes the cartilage. When moving, it acts as a shock absorber for the joints. The manipulation is painful, it is carried out by the doctor after the acute period has subsided. If conservative treatment is unsuccessful, endoprosthetics are performed.
Along with drug therapy, training using simulators and special devices (kinesitherapy) is prescribed. Ozone therapy has a positive effect on the condition of the knee. This substance is used externally, administered by subcutaneous or intramuscular injection, ozone-based ointment, cream. Manipulation stimulates blood circulation, increases the effect of chondroprotectors and glucocorticosteroids.
Modern nutritional supplements are in demand as an alternative to drugs for joint rehabilitation. Exercise and massage therapy are indicated. A set of special exercises improves blood circulation and nutrition of cartilage cells, increases the elasticity of ligaments.
Complications and prevention
Destroyed cartilage and deformed bones cannot be treated. In this situation, only surgery will help. No ointment or medicine can restore cartilage. Drugs can only stop the process of destruction of cartilage tissue.
Gonarthrosis develops gradually, sometimes the disease lasts for years. Without appropriate treatment, the patient's condition quickly deteriorates. The knee cannot function, serious complications appear:
- joint deformities;
- cosmetic defects - curvature of the limbs;
- infection with the bloodstream or lymph from other body sources;
- due to ligament weakness, dislocations and fractures are observed, even during normal walking;
- fusion of bones (ankylosis) occurs in the joint area, making movement impossible.
Complications develop if the patient does not see a doctor on time and the disease is advanced. Regular preventive examinations and timely treatment of general body diseases will help prevent the condition from getting worse and maintain the motor function of the limbs.



























































































